On examination you find:
- Speech – normal
- HMF – normal
- Cranial nerves – VA 6/9 both eyes; fields normal; movements normal; pupils react; optic discs hard to see clearly
- UL/LL – normal
- Gait – wobbly but otherwise normal
So what are your abnormal examination findings here?
Visual acuity is reduced bilaterally – make sure you have tested one eye at a time and that the patient wears glasses if needed (or use a pin hole if glasses not available).
Optic discs hard to see clearly – this is commonly written in notes when a junior doctor is not confident in their fundoscopy skills.
However, perhaps they are hard to see because the disc margins are actually blurred i.e. papilloedema.
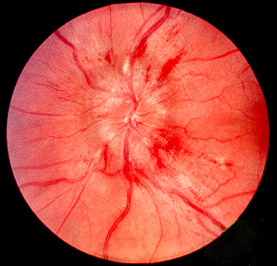
This is worrying in the context of headache and reduced visual acuity as it suggests raised intracranial pressure!
So now we are confident that this is not a primary but a secondary headache.
Lets look at our list of causes for secondary headache and see if we can complete the puzzle.
Vascular:
- Arterial (e.g. Subarachnoid haemorrhage): Doesn’t really sound like this, headache came on over a few days rather than thunderclap headache, no meningism.
- Venous (e.g. Cerebral venous sinus thrombosis): could be this, headache often worsens over a few days, can have associated visual disturbance, risk factors include dehydration as in this patient.
Infectious (e.g. Meningitis): No fever, neck stiffness or photophobia present to suggest this in this case.
Inflammatory (e.g. Giant cell arteritis): Our patient is not in the right age group for this, normally affects the over 50’s. Can lead to visual loss but often a unilateral headache with scalp tenderness and other systemic symptoms.
Too much CSF (e.g. Idiopathic intracranial hypertension (IIH)): often young women with recent weight gain, causes high pressure headache and can lead to visual loss
Too little CSF (e.g. meningeal cyst rupture or post-LP headache): low pressure headache, worse when standing up. Can get nausea, vomiting, neck pain, double vision.
So the top differential diagnoses for this patient, given the history and examination findings would be venous sinus thrombosis or IIH.
Note: People understandably worry about brain tumour in a patient with a headache suggestive of raised intracranial pressure. In fact, it is not common for a brain tumour to present with headache, normally presenting with seizures or focal neurology. Patients with brain tumours obviously can have headache but normally there is a more insidious onset with headache only when flow of CSF has become affected.
We need some imaging to help us. First choice for most of you would be CT head. This is fine but on its own would not help us rule out a CVST. We therefore need an additional CT venogram which uses contrast to visualise the venous system.
In this patient it may look something like this:

Diagnosis: Cerebral venous sinus thrombosis
This is an important cause of acute headache that is often missed. Can present as worsening headache over a few days but can also be a thunderclap headache.
Risk Factors: Dehydration, Pregnancy/ Post-partum, underlying malignancy, thrombophilias, hormonal contraception, chronic inflammatory disorders, local ear/nose infections.
For more information on assessment of acute headache, please watch our headache lecture here!
Leave a Reply